Core Tip: CFDA announced the new version of the GCP for Clinical Device Clinical Trial Quality Management on March 23, 2016. From the earliest order of the 2004 No. 5 to the 2012 draft, as a technical man engaged in medical device regulations and clinical trials for 15 years, he is well aware of the impact of the new version of the specification on the medical device industry. The author believes that the "Medical Device GCP" and the "new edition of the Medical Device Supervision and Management Regulations", the forthcoming "Medical Device Product Classification Catalogue" will form the three most important documents affecting the next 5-10 years of Chinese medical devices.
Foreword: The new edition of the "Quality Management Regulations for Clinical Instruments Clinical Trials" has a total of eleven chapters and 96 articles, which has undergone substantial changes than the original No. 5 of the seven chapters and twenty-nine. Covers the whole process of clinical trials of medical devices, including the design, implementation, monitoring, verification, inspection, and data collection, recording, analysis, and reporting of clinical trials. The Code sets out the responsibilities of the medical device clinical trial sponsors, clinical trial institutions, researchers and regulatory authorities, etc., from the protection of the rights and interests of the subjects and the regulation of clinical trials of medical devices, highlighting the role of the ethics committee and the informed consent of the subjects. Agree, increased the role of clinical monitoring, and emphasized risk control during clinical trials.
Oscar: This new edition of the clinical trial quality management guidelines for medical devices was released in August 2012. After three and a half years, the GCP boots for medical device clinical trial quality management standards finally fell.
Combined with the “Notice of the State Food and Drug Administration on the Self-inspection of Drug Clinical Trial Data (No. 169, 2015)†issued on July 22, 2015, the clinical trial of the drug as of January 20, 2016 The self-examination involved 1,622 varieties, 24 were not registered (1.5%), 958 was withdrawn (59%), and the clinical trial rate of drugs exceeded 60%, which was a heavy loss.
On February 27, 2016, CFDA announced that the hepatitis B virus core-associated antigen (HBcrAg) test kit for Japan's Fujirubeco Co., Ltd. was supervised by CFDA for clinical trial data of the registration application and found that it was in Shanghai. The public health clinical center, the Beijing You'an Hospital, and the Third Affiliated Hospital of the People's Liberation Army, the clinical trial data, such as the authenticity and other issues, and the announcement of the registration (No. 44, 2016), the storm of clinical data verification finally burned the medical The field of equipment.
Combined with the heavy release of this medical device GCP, the era of high requirements for clinical trials of medical devices has been grandly coming! ! ! Whether you like it or not, whether you are ready!
Medical Device Clinical Trial Quality Management Practice
Chapter I General
The first is to strengthen the management of clinical trials of medical devices, maintain the rights and interests of subjects in the clinical trials of medical devices, and ensure the standardization of clinical trial procedures for medical devices. The results are true, scientific, reliable and traceable, according to the Regulations on the Supervision and Administration of Medical Devices. ", develop this specification.
Oscar: New regulations add new science and traceability requirements. Traceability is the focus of follow-up clinical verification and self-examination, and is one of the most important clues in the verification storm of drug clinical trials started in 2015.
Article 2 The implementation of medical device clinical trials within the territory of the People's Republic of China shall follow this Code.
This specification covers the entire process of clinical trials of medical devices, including the design, implementation, monitoring, verification, and inspection of clinical trials, as well as the collection, recording, analysis, and reporting of data.
Oscar: Increased the requirements for the entire process of clinical trials of medical devices. The management of the entire process of clinical trials is also the biggest change in this GCP revision. And on this basis, the various aspects of the whole process have been refined.
Article 3 The term "medical device clinical trial" as used in this specification refers to the process of confirming or verifying the safety and effectiveness of a medical device to be applied for registration under normal use conditions in a medical device clinical laboratory certified by the qualification. .
Oscar: The new edition of the Code canceled the requirements for clinical trials of medical devices and clinical trials of medical devices. Because the current international practice of medical device supervision does not strictly distinguish clinical trials and clinical verification, and it is difficult to operate in actual work, it will be deleted.
Article 4 Clinical trials of medical devices shall follow legal principles, ethical principles and scientific principles.
Oscar: Not only ethics, but also law and science. However, the requirements for the law are not specific. Scientific principles are also relatively vague requirements. It is recommended that the officers inspecting the clinical trials need to comply with the supervisory regulations and the requirements of this GCP and other regulations.
Article 5 The food and drug supervision and administration department at or above the provincial level is responsible for the supervision and management of clinical trials of medical devices.
The health and family planning department strengthens the management of clinical trials of medical devices within the scope of their duties.
The food and drug supervision and administration department and the health and family planning department shall establish a medical device clinical trial quality management information notification mechanism, strengthen the third category of medical devices, medical devices listed in the national large-scale medical equipment configuration management products, and conduct clinical trial approval and corresponding clinical The information of the test supervision management data is reported.
Oscar: Increased supervision and management of provincial authorities and health and family planning authorities. Strengthened the third type of clinical trials of medical devices and the clinical trials and supervision of the national large-scale medical equipment configuration management products. Both types of medical device clinical trials will receive more regulation. The author believes that it will include the supervision of clinical verification and the supervision of the process. As for the form of supervision, we need to open our minds and think about it. The requirements for these two types of clinical trials will be higher, and the days of no configuration professionals will be more difficult.
Chapter II Preparation before clinical trials
Oscar: The second chapter of the new chapter from Article 6 to Article 12, “Pre-Clinical Test Preparation†consists of seven articles, which clarify the software and hardware conditions necessary for starting clinical trials of medical devices, and stipulate ethical review and administrative approval for clinical trials. Territorial filing requirements.
Article 6 The clinical trial of medical devices shall have sufficient scientific evidence and clear test objectives, and weigh the benefits and risks of the expected health of the subjects and the public. The expected benefits shall exceed the possible damage.
Article 7 Before the clinical trial, the sponsor shall complete the preclinical research of the medical device for testing, including product design (structural composition, working principle and mechanism of action, intended use and scope of application, applicable technical requirements) and quality inspection, animal testing. And risk analysis, etc., and the results should be able to support the clinical trial. The quality inspection results include the self-inspection report and the qualified product inspection inspection report issued within one year issued by a qualified inspection agency.
Oscar: Requires a product registration inspection report within one year. Animal testing and risk analysis are explicitly included here. It is no suspense to complete the risk management report before the clinic. The RAs are ready to go ahead and prepare for the day and night.
And for animal testing...
The old GCP has limited the requirements for animal testing: the test product is the first medical device used for implantation in the human body, and should have an animal test report of the product;
Other products that require animal testing to confirm the safety of the product to human clinical trials should also be submitted to the animal test report.
Little friends, the next time you apply for a clinical trial, different hospitals may discuss with you if you need an animal test report.
Article 8 Before the clinical trial, the sponsor shall prepare sufficient medical equipment for testing. The development of medical devices for testing shall comply with the relevant requirements of the applicable medical device quality management system.
Oscar: Test equipment needs to meet the requirements of the quality management system. The medical device for testing must meet the requirements of GMP and be determined again. Resent the partners who want to get products through OEMs! Of course, except for the innovative approval varieties!
Article 9 Clinical trials of medical devices shall be conducted in two or more clinical trial institutions for medical devices.
The selected testing institution shall be a medical device clinical testing institution certified by qualification, and the facilities and conditions shall meet the needs of safe and effective clinical trials. Researchers should have the expertise, qualifications, and competencies to undertake this clinical trial and be trained.
The administrative measures for the qualification certification of medical device clinical trial institutions shall be formulated separately by the State Food and Drug Administration and the National Health and Family Planning Commission.
Oscar: Medical device clinical trials will be identified separately. The draft of the "Measures for the Administration of Qualifications for Medical Device Clinical Trial Organizations" issued on July 20, 2015 has been published for more than half a year. It seems that the release of the official draft is also fast. The current department of the drug clinical trial institution can be used as a candidate for clinical trials of medical devices. Will the qualifications of clinical test institutions for medical devices be determined according to the department? Will the qualification license be one size fits all? Oscar is also drunk!
Article 10 Before the clinical trial, the sponsor and the clinical trial institution and the investigator shall reach a conclusion on the design of the trial, the quality control of the trial, the division of responsibilities in the trial, the costs associated with the clinical trial undertaken by the sponsor, and the principles of injury treatment that may occur during the trial. Written agreement.
Oscar: The scope of the written agreement with the clinical trial agency is defined. Do you have a small partner, the agreement being signed and the agreement to be signed? If the protocol template of some clinical trial institutions does not contain these complete contents, it needs to be revised as soon as possible!
Article 11 Clinical trials shall be approved by the ethics committee of the clinical trial organization of medical devices. The list of the third category of medical devices that need to be approved for clinical trials shall also be approved by the State Food and Drug Administration.
Oscar: Products approved for the catalog need to be approved by CFDA. On August 25, 2014, the first batch of approval catalogues (No. 14 of 2014) was released.
Article 12 Before the clinical trial, the sponsor shall file with the food and drug supervision and administration department of the local province, autonomous region or municipality directly under the Central Government for the record.
The food and drug supervision and administration department that accepts the record shall notify the food and drug supervision and administration department at the same level as the location of the clinical trial institution and the competent department of health and family planning.
Oscar: All clinical trials need to be filed. Note that it is the record before the test, that is, the clinical trial can only be started after the completion of the record. The filing status will be notified to the location of the institution conducting the clinical trial. Xiaobian is thinking, will they check the flight during the test? Is it going to be, or will it? ? Especially the third category and included in the national large-scale medical equipment configuration management products! Then, not only the clinical trial results should be standardized, but the process can be reviewed and standardized at any time.
Chapter III Subject Rights Protection
Article 13 Clinical trials of medical devices shall follow the ethical guidelines established by the Helsinki Declaration of the World Medical Congress.
Article 14 Ethical review and informed consent are the main measures to protect the rights and interests of the subjects. The parties involved in the clinical trial shall bear corresponding ethical responsibilities in accordance with their respective duties in the trial.
Article 15 The sponsor shall avoid undue influence or misleading of clinical trial participants or related parties such as subjects, clinical trial institutions and researchers.
Clinical trial institutions and researchers should avoid undue influence or misleading of clinical trial participants or related parties such as subjects and sponsors.
Article 16 Sponsors, clinical trial institutions and researchers shall not exaggerate the compensation measures involved in clinical trials and mislead subjects to participate in clinical trials.
Oscar: Do not exaggerate or mislead parties.
Article 17 Before the clinical trial, the sponsor shall submit the following documents to the ethics committee through the medical device clinical trial management department of the researcher and the clinical trial institution:
(1) clinical trial plan;
(2) The researcher's manual;
(3) the text of the informed consent form and any other written materials provided to the subject;
(iv) procedural documents for recruiting and advertised to the subject;
(5) The text of the case report form;
(6) Self-inspection report and product registration inspection report;
(7) The resume, professional expertise, ability, training and other documents that can prove his or her qualifications;
(8) The facilities and conditions of the clinical trial institution can satisfy the review of the trial;
(9) A statement that the development of the medical device for testing meets the relevant requirements of the applicable medical device quality management system;
(10) Other documents related to ethical review.
The ethics committee should uphold the principles of ethics and science to review and supervise the implementation of clinical trials.
Oscar: The information on the ethics submitted here is relatively complete. The ethical data process of some hospitals needs to be modified with reference to this requirement.
First: Before the clinical trial, the sponsor shall complete the preclinical research of the medical device for testing, including product design (structural composition, working principle and mechanism of action, intended use and scope of application, applicable technical requirements). And quality testing, animal testing, and risk analysis, and the results should be able to support the clinical trial." There is no explicit requirement for submission in the ethical application process. Will the follow-up of clinical trials require attention to the completion of this part of the work? Although there is no explicit provision, the clinical trial institution said that it is not allowed to find the sponsor.
Second: the principle of “scientific†review required by this article. This means that clinical trial institutions need to review the “scientific†nature of the ethical review process. Clinical trial institutions are very professional in protecting ethics and subject rights, and for the grasp of "scientific", it is estimated that many experimental institutions should start research. After all, "scientific" is one of the three principles of this GCP Article 4 "Clinical trials of medical devices should follow legal principles, ethical principles, and scientific principles." In the full text of this GCP, "science" appears 12 times, and the judgment of the scientific review is the main responsibility of the ethics committee. In Article 93, the definition is given as: an ethics committee, which refers to an independent institution set up by a clinical trial institution to review the scientific and ethical nature of clinical trials of medical devices. Leaders of the ethics committee, are you also starting to be a bit big and stressful? !
Article 18 In the case of any of the following conditions during the clinical trial, the investigator shall promptly report to the clinical trial management department of the clinical trial institution, and notify the sponsor and the report ethics committee in time:
(1) Serious adverse events;
(2) Progress report, including safety summary and deviation report;
(3) Any amendments to the approved documents of the ethics committee shall not affect the rights, safety and health of the subjects, or insubstantial changes that are not related to the purpose or end point of the clinical trial, without prior reporting, but shall be notified in writing afterwards;
(4) requesting the restoration of clinical trials after suspension, termination or suspension;
(5) Scientific trial protocol deviations affecting the subject's rights, safety and health or clinical trials, including request deviation and reporting deviation.
In order to protect the rights, safety and health of the subjects, if the deviation occurred in an emergency situation cannot be reported in time, it shall be reported in writing as soon as possible in accordance with relevant regulations.
Article 19 In the course of clinical trials, if the revision of clinical trial plan and informed consent documents, requests for deviation, and restoration of suspended clinical trials, the written approval of the ethics committee shall be followed.
Oscar: Please note that it is approved before proceeding.
Article 20: It is necessary to avoid the selection of minors, pregnant women, the elderly, mentally handicapped persons, and patients in critical situations of life as subjects; if it is necessary to select, it shall comply with the relevant additional requirements put forward by the ethics committee. The test is specifically designed for its health and should be beneficial to its health.
Article 21 Before the subject participates in the clinical trial, the investigator shall fully explain the details of the clinical trial to the subject or the guardian of the person without civil capacity or the person with limited capacity for civil conduct, including known and foreseeable Risks and possible adverse events, etc. After full and detailed explanation, the subject or his or her guardian signs the name and date on the informed consent form, and the investigator must also sign the name and date on the informed consent form.
Article 22 The informed consent form shall generally include the following contents and a description of the matters:
(1) the name of the researcher and related information;
(2) the name of the clinical trial institution;
(3) The name, purpose, method and content of the test;
(4) The test process and time limit;
(5) The source of funds for the trial and possible conflicts of interest;
(vi) Possible benefits and known, foreseeable risks and possible adverse events of the intended subject;
(7) Information on alternative treatment methods available to the subject and their potential benefits and risks;
(v) when needed, indicating that the subject may be assigned to a different group of trials;
(9) Subjects participating in the trial shall be voluntary and shall have the right to withdraw at any stage of the trial without discrimination or retaliation, and their medical treatment and rights shall not be affected;
(10) The personal data that informs the participants to participate in the trial is confidential, but the ethics committee, the food and drug supervision and administration department, the health and family planning authority or the sponsor may, in accordance with the prescribed procedures, refer to the personal data of the participants participating in the trial;
(11) Subjects may receive treatment and financial compensation in the event of injury associated with the test;
(12) Subjects may keep abreast of the information related to them during the trial;
(13) Free medical treatment items and other related subsidies that the subject may receive during the trial.
Informed consent should be in a language and script that the subject or guardian can understand. Informed consent should not contain content that would cause the subject to waive legal rights and to waive the responsibility of the clinical trial institution and the investigator, sponsor, or agent.
Oscar: The informed consent form templates of the general clinical trial institutions basically meet the requirements of this article. However, as soon as possible, refer to the "Notice of the General Administration on the publication of the "National Medical Device Clinical Trial Application and Approval Form" and other six documents (No. 58 of 2016), Annex 2. Model Informed Consent Form. The modified place was modified early.
Article 23 The obtaining of informed consent shall also meet the following requirements:
(1) For a non-behaving subject, if the ethics committee agrees in principle and the investigator believes that the subject participates in the clinical trial in its own interest, it can also enter the clinical trial, but the signature should be signed and signed by the guardian before the trial. Date.
(2) When the subject or his guardian has no reading ability, a witness should be present in the informed process. After the informed consent is given, the witness reads the informed consent and the oral informed content is consistent with the subject or After the guardian’s head agrees, the witness signs and dated the informed consent, and the witness’s signature and the investigator’s signature should be on the same day.
(3) If a minor is a subject, he or she shall obtain the informed consent of the guardian and sign the informed consent form. If the minor can express his or her intention to participate in the trial, he or she shall also obtain his or her consent.
(4) If the important information related to the medical device for trial or the clinical impact other than the expected clinical impact is found, the relevant content of the informed consent form shall be revised. After the revised informed consent form is approved by the ethics committee, it shall be re-established by the subject or its guardian. Signature confirmation.
Article 24 The informed consent form shall indicate the date of the enactment or the date of the revised version. If the informed consent form has been revised during the trial, the revised informed consent form must be approved by the ethics committee again. After the revised informed consent form is reported to the clinical trial facility, all subjects who have not completed the trial process should sign a newly revised informed consent if they are affected.
Oscar: A revised informed consent form, after a revised version of the informed consent form is reported to the clinical trial facility, all subjects who have not completed the trial process should sign a new revised informed consent if affected. If affected, a new version of the informed consent form will need to be signed again.
Article 25 Subjects have the right to withdraw at any stage of the clinical trial and do not bear any financial responsibility.
Chapter IV Clinical Trial Program
Article 26 To carry out clinical trials of medical devices, the sponsor shall organize scientific and reasonable clinical trial programs according to the types, risks and intended uses of the medical devices for testing.
Article 27: For new products that have not been approved for listing at home and abroad, the safety and performance have not been confirmed by medical treatment. The clinical trial plan should be designed with a small sample feasibility test. After the initial confirmation of its safety, according to the statistics The study requires the determination of the sample size for subsequent clinical trials.
Oscar: It is proposed that for new products, safety and performance have not been medically proven, clinical trial design should first carry out a small sample feasibility test to initially determine its safety. This is similar to the phase II clinical trial requirements for drugs. Then the following two situations, the partners should pay attention to:
First: If a small sample feasibility test is to be carried out, then this small sample test should also be done in full accordance with the requirements of the GCP, program, informed consent, ethics committee approval, clinical implementation, statistics, reporting, and then draw conclusions --- Then, determine the final clinical sample size, the ethics committee approves again, and then informed consent to enter the formal clinical. A little bit around, but also a little challenge; is it going to be done twice?
Second: Can a small sample of clinical trials be approved without an ethics committee? Should not be! However, how can the ethics committee approve such projects? Little friends have to open their minds and think about ways!
Article 28 The clinical trial plan for medical devices shall include the following contents:
(1) General information;
(2) Background information on clinical trials;
(3) The purpose of the test;
(4) Experimental design;
(5) Safety evaluation methods;
(6) Method of effectiveness evaluation;
(7) Statistical considerations;
(8) Provisions for the revision of the clinical trial plan;
(9) Provisions on reports of adverse events and device defects;
(10) Direct access to source data and documents;
(11) Ethical issues and explanations related to clinical trials and the text of informed consent;
(12) Data processing and record keeping;
(13) Finance and insurance;
(14) The test results are published.
Some of the above may be included in other relevant documents of the program such as the researcher's manual. The specific information of the clinical trial institution, the publication of the test results, financial and insurance can be expressed in the test plan, or an additional agreement can be made.
Oscar: Added some requirements and gave a new solution template different from the original GCP. Be sure to refer to the General Administration's circular on the publication of the six documents including the “Application for Approval and Approval of Medical Device Clinical Trial Examinations†(No. 58 of 2016) Annex 4. Model of clinical trials for medical devices.
Article 29 Multi-center clinical trials are conducted by multiple investigators in the same clinical trials in different clinical trial institutions. The design and implementation of its test plan should include at least the following:
(1) The trial protocol is formulated by the sponsor organization and discussed by the clinical trial institutions and researchers, and the investigator of the lead clinical unit is the coordinating researcher;
(2) Coordinating the researcher to be responsible for the coordination of work among the clinical trial institutions during the clinical trial, organizing the investigator meeting in the pre-, mid-, and post-clinical trials, and cooperating with the sponsor for the implementation of the entire trial;
(3) Each clinical trial institution shall, in principle, carry out and end clinical trials at the same time;
(4) Reasons for the sample size and distribution of each clinical trial institution and the requirements for statistical analysis;
(5) The plan and training record requirements for the trial training of the sponsor and the clinical trial institution;
(6) Establish procedures for the transmission, management, verification and inquiry of test data, and specifically require that the relevant data of the trial data of each clinical trial institution should be managed and analyzed centrally by the lead unit;
(7) After the end of the multi-center clinical trial, the researchers in each clinical trial institution shall issue a summary of the clinical trial, together with the medical report form, and submit it to the coordinating researcher to complete the summary report.
Oscar: This article is a detailed requirement for a multi-center clinical trial. This includes requiring clear lead units and coordinating researchers. Note that multicenter refers to three or more centers. The definition of Article 93 is very clear: “Multi-center clinical trials refer to clinical trials conducted in more than three (including three) clinical trial institutions in accordance with the same clinical trial protocol.â€. That is, two clinical trial institutions are not multi-center.
Chapter V Ethics Committee Responsibilities
Oscar: The fifth chapter is the new chapter. There are eight ethics committee responsibilities, which mainly explain the composition, construction, working procedures, responsibilities, and points that need to be considered. It is clear that the ethical review should include a scientific review of the clinical trial. While giving the ethics committee the right to consent to clinical trials, it also gives them the power to suspend or terminate clinical trials, effectively protecting the rights of the subjects.
Article 30 The ethics committee of a medical device clinical trial institution shall consist of at least five members, including medical professionals and non-medical professionals, which shall have members of different genders. At least one of the non-medical professional members is a legal worker and one is a person outside the clinical trial institution. Members of the Ethics Committee shall have qualifications or experience in assessing and evaluating the scientific, medical, and ethical aspects of the clinical trial. All members should be familiar with the ethical guidelines and relevant regulations for clinical trials of medical devices and comply with the ethics committee's charter.
Article 31 The Medical Device Ethics Committee shall abide by the ethical guidelines of the Helsinki Declaration of the World Medical Congress and the provisions of the food and drug supervision and administration department, establish corresponding working procedures and form documents, and perform duties in accordance with the working procedures.
Members of the ethics committee independent of the investigator and sponsor have the right to express their opinions and participate in the voting on the trial.
Article 32 The ethics committee shall convene a meeting in advance, and the number of participants in the review and voting shall not be less than five. Any decision made by the ethics committee shall be passed by more than half of the members of the ethics committee.
Researchers can provide information about any aspect of the trial, but should not participate in the review, vote, or comment.
The ethics committee may invite experts from relevant fields to participate in the review of certain special trials.
Article 33 The ethics committee shall strictly consider the test plan and related documents from the perspective of safeguarding the rights and interests of the subjects, and shall focus on the following contents:
(1) The qualifications, experience, and sufficient time of the investigator to participate in the clinical trial.
(2) Whether the staffing of the clinical testing institution and the equipment conditions meet the test requirements.
(3) The degree of risk that the subject may be exposed to is appropriate compared to the expected benefit of the trial.
(4) Whether the trial plan fully considers the ethical principles and whether it is scientific, including whether the research purpose is appropriate, whether the subject's rights are protected, whether other people may be exposed to risks, and whether the subject is selected scientifically.
(5) The method of enrolling the subject, whether the information provided to the subject or his or her guardian about the test is complete, whether the subject understands, and whether the method of obtaining the informed consent is appropriate; if necessary, the ethics committee should organize The test population representative tests the comprehensibility of the data and assesses whether the informed consent is appropriate. The results of the assessment should be documented and saved to 10 years after the end of the clinical trial.
(6) Whether the treatment and insurance measures given are sufficient if the subject has suffered injury or death related to the clinical trial.
(7) Whether the amendments proposed to the test plan are acceptable.
(8) Whether it is possible to periodically analyze and evaluate the possible hazards to the subjects during the clinical trial.
(9) Deviations from the test protocol may affect the subject's rights, safety and health, or affect the scientific and completeness of the test, and whether it is acceptable.
Article 34 The ethical review of a multi-center clinical trial shall be undertaken by the ethics committee of the lead unit to establish a collaborative review process to ensure consistency and timeliness of the review.
Before the start of the trial in each clinical trial institution, the ethics committee of the lead unit shall be responsible for reviewing the ethical rationality and scientificity of the trial protocol. The ethics committees of other clinical trial institutions participating in the trial may adopt the conference review on the premise of accepting the review opinions of the ethics committee of the lead unit. Or the method of document review, review the feasibility of the trial in this clinical trial institution, including the qualifications and experience of the investigator, equipment and conditions, etc., generally no longer modify the design of the trial scheme, but has the right not to approve Tested in its clinical trial facility.
Oscar: The multi-center ethical review is based on the review of the lead unit ethics committee. The ethics committees participating in other clinical trial institutions generally do not propose amendments to the trial protocol, but have the right not to approve trials in their clinical trial facilities. To some extent, the ethical review of a multicenter clinical trial may be more efficient than the ethical review of the 2 centers in terms of a coordinated approach. For the 2-center clinical trial, there is no clear definition.
Article 35 After receiving an application for a clinical trial of medical devices, the ethics committee shall convene a meeting to review and discuss, issue written opinions and seals, and attach a list of personnel attending the meeting, the profession, and the signature of the person. The opinions of the ethics committee can be:
(1) agree;
(2) agreeing with the necessary modifications;
(3) disagree;
(4) Suspension or termination of the approved test.
Article 36 The ethics committee shall follow up and supervise the clinical trials of the clinical trial institution and find that the subject's rights and interests cannot be guaranteed. The clinical trial may be suspended or terminated at any time in writing.
Suspended clinical trials may not be resumed without the consent of the ethics committee.
Article 37 The ethics committee shall retain all relevant records until at least 10 years after the completion of the clinical trial.
Oscar: All relevant records of the Ethics Committee are required to remain for 10 years. For the record keeping time of the applicants and other units, this GCP has not made explicit provisions.
Chapter VI Sponsor's Responsibilities
Oscar: Chapter VI “Sponsor's Responsibilities†consists of 21 articles. It specifies the main responsibilities and documents provided by the sponsors, and also stipulates the selection, scope of work and commitment of the auditors and inspectors. The responsibility clarifies that the sponsor is responsible for the authenticity and reliability of the clinical trial and the safety of the clinical trial of the medical device used for the trial.
Article 38 The sponsor is responsible for initiating, applying, organizing, and supervising clinical trials, and is responsible for the authenticity and reliability of clinical trials. The sponsor is usually a medical device manufacturer. Where the sponsor is an overseas institution, an agent shall be appointed within the territory of China.
Oscar: The new version of the regulations unifies the “implementer†of the original regulations to the “sponsorâ€. It also clarifies that the sponsor is responsible for the authenticity and reliability of the clinical trial, which is exactly the same as the sponsor is the direct person in charge of the quality of the medical device product.
Article 39 The sponsor is responsible for organizing the development and revision of the researcher's manual, clinical trial protocol, informed consent form, case report form, relevant standard operating procedures and other relevant documents, and is responsible for organizing the training necessary for clinical trials.
Article 40 The sponsor shall select the testing institution and its researcher in the medical device clinical testing institution certified by the qualification according to the characteristics of the medical device for testing. The sponsor should provide the clinical investigator and the investigator with the most up-to-date investigator's manual and other relevant documents before deciding to sign a clinical trial agreement with the clinical trial facility for the decision to accept the clinical trial.
Article 41 The researcher's manual shall include the following main contents:
(1) Basic information of the sponsor and the researcher;
(2) A summary description of the medical device for testing;
(3) Supporting the summary and evaluation of the intended use of the medical device for trial use and the rationale for the design of the clinical trial;
(4) A statement that the manufacture of the medical device for testing conforms to the requirements of the applicable medical device quality management system.
Article 42 The sponsor shall not exaggerate the mechanism and efficacy of the medical device for testing in the formulation of the clinical trial program.
Article 43 In the course of clinical trials, when the sponsor obtains important information affecting the clinical trial, the researcher's manual and related documents shall be revised in time, and submitted to the ethics committee for review by the medical device clinical trial management department of the clinical trial institution. agree.
Article 44 The sponsor shall reach a written agreement with the clinical trial institution and the investigator on the following matters:
(1) Implement clinical trials in accordance with relevant laws and regulations and clinical trial programs, and accept audits, verifications and inspections;
(2) Following the data recording and reporting procedures;
(3) retaining the basic documents related to the trial no less than the statutory time until the sponsor notifies the clinical trial institution and the investigator that the document is no longer needed;
(四)申办者得到伦ç†å§”员会批准åŽï¼Œè´Ÿè´£å‘ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…æ供试验用医疗器械,并确定其è¿è¾“æ¡ä»¶ã€å‚¨å˜æ¡ä»¶ã€å‚¨å˜æ—¶é—´ã€æœ‰æ•ˆæœŸç‰ï¼›
(五)试验用医疗器械应当质é‡åˆæ ¼ï¼Œå…·æœ‰æ˜“于识别ã€æ£ç¡®ç¼–ç 以åŠè´´æœ‰â€œè¯•éªŒç”¨â€çš„ç‰¹æ®Šæ ‡è¯†ï¼Œå¹¶æŒ‰ç…§ä¸´åºŠè¯•éªŒæ–¹æ¡ˆè¦æ±‚进行适当包装和ä¿å˜ï¼›
(å…)申办者应当制定临床试验质é‡æŽ§åˆ¶ç›¸å…³çš„æ ‡å‡†æ“作规程,如试验用医疗器械的è¿è¾“ã€æŽ¥æ”¶ã€å‚¨å˜ã€åˆ†å‘ã€å¤„ç†ã€å›žæ”¶ç‰ï¼Œä¾›ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…éµå¾ªã€‚
Oscar:第四åå››æ¡æ–°å¢žä¹¦é¢åè®®è¦æ±‚。在本GCP的第åæ¡ä¸ï¼Œè¦æ±‚ç¾è®¢ä¹¦é¢å议。“第åæ¡ ä¸´åºŠè¯•éªŒå‰ï¼Œç”³åŠžè€…ä¸Žä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“å°±è¯•éªŒè®¾è®¡ã€è¯•éªŒè´¨é‡æŽ§åˆ¶ã€è¯•éªŒä¸çš„èŒè´£åˆ†å·¥ã€ç”³åŠžè€…承担的临床试验相关费用以åŠè¯•éªŒä¸å¯èƒ½å‘生的伤害处ç†åŽŸåˆ™ç‰è¾¾æˆä¹¦é¢å议。â€ã€‚至于ç¾ä¸€ä»½å议或者ç¾ä¸¤ä»½å议,这就è¦çœ‹çœ‹å®˜ä½ 自己了,å¦å¤–,医院的å议模æ¿ä¹Ÿéœ€è¦ä¿®æ”¹äº†ã€‚
第四åäº”æ¡ ç”³åŠžè€…å¯¹è¯•éªŒç”¨åŒ»ç–—å™¨æ¢°åœ¨ä¸´åºŠè¯•éªŒä¸çš„安全性负责。当å‘现å¯èƒ½å½±å“å—试者安全或者试验实施å¯èƒ½æ”¹å˜ä¼¦ç†å§”员会对继ç»è¯•éªŒçš„批准情况时,申办者应当立å³é€šçŸ¥æ‰€æœ‰ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…ï¼Œå¹¶åšå‡ºä½œå‡ºç›¸åº”处ç†ã€‚
第四åå…æ¡ ç”³åŠžè€…å†³å®šæš‚åœæˆ–者终æ¢ä¸´åºŠè¯•éªŒçš„,应当在55日内通知所有临床试验机构医疗器械临床试验管ç†éƒ¨é—¨ï¼Œå¹¶ä¹¦é¢è¯´æ˜Žç†ç”±ã€‚临床试验机构医疗器械临床试验管ç†éƒ¨é—¨åº”当åŠæ—¶é€šçŸ¥ç›¸åº”çš„ç ”ç©¶è€…ã€ä¼¦ç†å§”员会。对暂åœçš„临床试验,未ç»ä¼¦ç†å§”员会åŒæ„,ä¸å¾—æ¢å¤ã€‚临床试验结æŸåŽï¼Œç”³åŠžè€…应当书é¢å‘ŠçŸ¥å…¶æ‰€åœ¨åœ°çœã€è‡ªæ²»åŒºã€ç›´è¾–市食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨ã€‚
第四åä¸ƒæ¡ ç”³åŠžè€…åº”å½“ä¿è¯å®žæ–½ä¸´åºŠè¯•éªŒçš„æ‰€æœ‰ç ”ç©¶è€…ä¸¥æ ¼éµå¾ªä¸´åºŠè¯•éªŒæ–¹æ¡ˆï¼Œå‘çŽ°ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…ä¸éµä»Žæœ‰å…³æ³•å¾‹æ³•è§„ã€æœ¬è§„范和临床试验方案的,应当åŠæ—¶æŒ‡å‡ºå¹¶äºˆä»¥çº æ£ï¼›å¦‚情况严é‡æˆ–者æŒç»ä¸æ”¹ï¼Œåº”当终æ¢è¯•éªŒï¼Œå¹¶å‘临床试验机构所在地çœã€è‡ªæ²»åŒºã€ç›´è¾–市食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨å’Œå›½å®¶é£Ÿå“è¯å“监ç£ç®¡ç†æ€»å±€æŠ¥å‘Šã€‚
第四åå…«æ¡ ç”³åŠžè€…åº”å½“ä¸ºå‘生与临床试验相关的伤害或者æ»äº¡çš„å—试者承担治疗的费用以åŠç›¸åº”çš„ç»æµŽè¡¥å¿ï¼Œä½†åœ¨è¯Šç–—活动ä¸ç”±åŒ»ç–—机构åŠå…¶åŒ»åŠ¡äººå‘˜è¿‡é”™é€ æˆçš„æŸå®³é™¤å¤–。
第四åä¹æ¡ 申办者应当对临床试验承担监查责任,并选择符åˆè¦æ±‚的监查员履行监查èŒè´£ã€‚
监查员人数以åŠç›‘查的次数å–决于临床试验的å¤æ‚程度和å‚与试验的临床试验机构数目。
Oscar:本GCPä¸ï¼Œæ–°å¢žäº†å¯¹äºŽç›‘查员的è¦æ±‚,并且规定由申办者承担监查责任并选择监查员。这进一æ¥æ高和规范了医疗器械临床试验的è¦æ±‚。申办者需è¦è‡ªå·±åŸ¹å…»åˆæ ¼çš„监查员或者更多è¦ä¾èµ–专业的CRO机构如龙德医疗器械æœåŠ¡é›†å›¢è¿™æ ·çš„专业的医疗器械临床试验åˆåŒç ”究组织了。
第五åæ¡ ç›‘æŸ¥å‘˜åº”å½“æœ‰ç›¸åº”çš„ä¸´åºŠåŒ»å¦ã€è¯å¦ã€ç”Ÿç‰©åŒ»å¦å·¥ç¨‹ã€ç»Ÿè®¡å¦ç‰ç›¸å…³ä¸“业背景,并ç»è¿‡å¿…è¦çš„培è®ï¼Œç†Ÿæ‚‰æœ‰å…³æ³•è§„和本规范,熟悉有关试验用医疗器械的éžä¸´åºŠå’ŒåŒç±»äº§å“临床方é¢çš„ä¿¡æ¯ã€ä¸´åºŠè¯•éªŒæ–¹æ¡ˆåŠå…¶ç›¸å…³çš„文件。
Oscar:对于监查员有专业åŠç›¸å…³èƒŒæ™¯çš„è¦æ±‚,监查员的这些背景è¦åŽ»éƒ½éœ€è¦è¢«è®°å½•ä¸‹æ¥å’Œç•™å˜ç›¸åº”çš„è¯æ®ã€‚
第五åä¸€æ¡ ç›‘æŸ¥å‘˜åº”å½“éµå¾ªç”±ç”³åŠžè€…åˆ¶å®šçš„è¯•éªŒç”¨åŒ»ç–—å™¨æ¢°ä¸´åºŠè¯•éªŒç›‘æŸ¥æ ‡å‡†æ“作规程,ç£ä¿ƒä¸´åºŠè¯•éªŒæŒ‰ç…§æ–¹æ¡ˆå®žæ–½ã€‚具体èŒè´£åŒ…括:
(一)在试验å‰ç¡®è®¤ä¸´åºŠè¯•éªŒæœºæž„已具有适当的æ¡ä»¶ï¼ŒåŒ…括人员é…备与培è®ç¬¦åˆè¦æ±‚,实验室设备é½å…¨ã€å·¥ä½œæƒ…况良好,预期有足够数é‡çš„å—试者,å‚ä¸Žç ”ç©¶äººå‘˜ç†Ÿæ‚‰è¯•éªŒè¦æ±‚;。
(二)在试验å‰ã€ä¸ã€åŽæœŸç›‘æŸ¥ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…æ˜¯å¦éµå¾ªæœ‰å…³æ³•è§„ã€æœ¬è§„范和临床试验方案;
(三)确认æ¯ä½å—试者在å‚与临床试验å‰ç¾ç½²çŸ¥æƒ…åŒæ„书,了解å—试者的入选情况以åŠè¯•éªŒçš„è¿›å±•çŠ¶å†µï¼›å¯¹ç ”ç©¶è€…æœªèƒ½åšåˆ°çš„éšè®¿ã€æœªè¿›è¡Œçš„试验ã€æœªåšçš„检查,以åŠæ˜¯å¦å¯¹é”™è¯¯ã€é—æ¼åšå‡ºçº æ£ç‰ï¼Œåº”当清楚ã€å¦‚实记录;对修订的知情åŒæ„书,确认未结æŸä¸´åºŠè¯•éªŒæµç¨‹å¹¶å—å½±å“çš„å—试者é‡æ–°ç¾ç½²ï¼›
(四)确认所有病例报告表填写æ£ç¡®ï¼Œå¹¶ä¸ŽåŽŸå§‹èµ„料一致;所有错误或者é—æ¼å‡å·²æ”¹æ£æˆ–者注明,ç»ç ”究者ç¾å并注明日期;æ¯ä¸€è¯•éªŒçš„ç—…ç§ã€ç—…例总数和病例的性别ã€å¹´é¾„ã€æ²»ç–—效果ç‰å‡åº”当确认并记录;
(五)确认å—试者退出临床试验或者ä¸ä¾ä»ŽçŸ¥æƒ…åŒæ„书规定è¦æ±‚çš„æƒ…å†µè®°å½•åœ¨æ¡ˆï¼Œå¹¶ä¸Žç ”ç©¶è€…è®¨è®ºæ¤ç§æƒ…况;
(å…)确认所有ä¸è‰¯äº‹ä»¶ã€å¹¶å‘症和其他器械缺陷å‡è®°å½•åœ¨æ¡ˆï¼Œä¸¥é‡ä¸è‰¯äº‹ä»¶å’Œå¯èƒ½å¯¼è‡´ä¸¥é‡ä¸è‰¯äº‹ä»¶çš„器械缺陷在规定时间内åšå‡ºä½œå‡ºæŠ¥å‘Šå¹¶è®°å½•åœ¨æ¡ˆï¼›
ï¼ˆä¸ƒï¼‰ç›‘æŸ¥è¯•éªŒç”¨åŒ»ç–—å™¨æ¢°æ ·å“的供给ã€ä½¿ç”¨ã€ç»´æŠ¤ä»¥åŠè¿è¾“ã€æŽ¥æ”¶ã€å‚¨å˜ã€åˆ†å‘ã€å¤„ç†ä¸Žå›žæ”¶ï¼›
(八)监ç£ä¸´åºŠè¯•éªŒè¿‡ç¨‹ä¸ç›¸å…³è®¾å¤‡çš„å®šæœŸç»´æŠ¤å’Œæ ¡å‡†ï¼›
(ä¹ï¼‰ç¡®ä¿ç ”究者收到的所有临床试验相关文件为最新版本;
(å)æ¯æ¬¡ç›‘查åŽåº”当书é¢æŠ¥å‘Šç”³åŠžè€…,报告应当包括监查员姓åã€ç›‘查日期ã€ç›‘查时间ã€ç›‘查地点ã€ç›‘查内容ã€ç ”究者姓åã€é¡¹ç›®å®Œæˆæƒ…况ã€å˜åœ¨çš„问题ã€ç»“论以åŠå¯¹é”™è¯¯ã€é—æ¼åšå‡ºçš„çº æ£ç‰ã€‚
Oscar:本æ¡åˆ—出了监查员的主è¦èŒè´£ã€‚相应的,监查员工作的SOP和相关的表å•è®°å½•éƒ½éœ€è¦åšå‡ºä¸“ä¸šçš„å‡†å¤‡ï¼Œè¿™æ ·çš„ç›‘æŸ¥å‘˜çš„å·¥ä½œæ‰èƒ½æ»¡è¶³æœ¬GCPçš„è¦æ±‚。å„ä½çœ‹å®˜çš„监查员的èŒè´£å’ŒSOP涵盖了这些内容å—?
第五åäºŒæ¡ ç”³åŠžè€…ä¸ºä¿è¯ä¸´åºŠè¯•éªŒçš„è´¨é‡ï¼Œå¯ä»¥ç»„织独立于临床试验ã€å¹¶å…·æœ‰ç›¸åº”培è®å’Œç»éªŒçš„æ ¸æŸ¥å‘˜å¯¹ä¸´åºŠè¯•éªŒå¼€å±•æƒ…å†µè¿›è¡Œæ ¸æŸ¥ï¼Œè¯„ä¼°ä¸´åºŠè¯•éªŒæ˜¯å¦ç¬¦åˆè¯•éªŒæ–¹æ¡ˆçš„è¦æ±‚。
æ ¸æŸ¥å¯ä»¥ä½œä¸ºç”³åŠžè€…临床试验质é‡ç®¡ç†å¸¸è§„工作的一部分,也å¯ä»¥ç”¨äºŽè¯„估监查活动的有效性,或者针对严é‡çš„或者åå¤çš„临床试验方案å离ã€æ¶‰å«Œé€ å‡ç‰æƒ…å†µå¼€å±•æ ¸æŸ¥ã€‚
Oscar:除了监查员之外,申办者å¯ä»¥å†å®‰æŽ’æ ¸æŸ¥å‘˜å¼€å±•å·¥ä½œï¼Œè¯„ä¼°ä¸´åºŠè¯•éªŒæ˜¯å¦ç¬¦åˆä¸´åºŠè¯•éªŒæ–¹æ¡ˆçš„è¦æ±‚ã€‚å½“ç„¶ï¼Œæ ¸æŸ¥å‘˜ä¹Ÿéœ€è¦å‡†å¤‡ç›¸å…³çš„æ ¸æŸ¥æ–¹æ¡ˆã€æ ¸æŸ¥ç¨‹åºå’Œç›¸å…³çš„SOP。
第五åä¸‰æ¡ æ ¸æŸ¥å‘˜åº”å½“æ ¹æ®ä¸´åºŠè¯•éªŒçš„é‡è¦æ€§ã€å—试者数é‡ã€ä¸´åºŠè¯•éªŒçš„类型以åŠå¤æ‚性ã€å—试者风险水平ç‰åˆ¶å®šæ ¸æŸ¥æ–¹æ¡ˆå’Œæ ¸æŸ¥ç¨‹åºã€‚
第五åå››æ¡ å¯¹äºŽä¸¥é‡ä¸è‰¯äº‹ä»¶å’Œå¯èƒ½å¯¼è‡´ä¸¥é‡ä¸è‰¯äº‹ä»¶çš„器械缺陷,申办者应当在获知åŽ5个工作日内å‘所备案的食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨å’ŒåŒçº§å«ç”Ÿè®¡ç”Ÿä¸»ç®¡éƒ¨é—¨æŠ¥å‘Šï¼ŒåŒæ—¶åº”当å‘å‚ä¸Žè¯•éªŒçš„å…¶ä»–ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…é€šæŠ¥ï¼Œå¹¶ç»å…¶åŒ»ç–—器械临床试验管ç†éƒ¨é—¨åŠæ—¶é€šçŸ¥è¯¥ä¸´åºŠè¯•éªŒæœºæž„的伦ç†å§”员会。
第五åäº”æ¡ ç”³åŠžè€…è‹¥é‡‡ç”¨ç”µå临床数æ®åº“或者远程电å临床数æ®ç³»ç»Ÿï¼Œåº”当确ä¿ä¸´åºŠæ•°æ®çš„å—控ã€çœŸå®žï¼Œå¹¶å½¢æˆå®Œæ•´çš„验è¯æ–‡ä»¶ã€‚
Oscar:对于采用电å临床数æ®åº“或者远程电å临床数æ®ç³»ç»Ÿçš„,软件需è¦å®Œæˆç›¸åº”的验è¯ï¼ŒåŒ…括数æ®çš„å—控性和真实性,包括必è¦çš„电åç¾å的控制ç‰éƒ½éœ€è¦è€ƒè™‘。
第五åå…æ¡ å¯¹äºŽå¤šä¸å¿ƒä¸´åºŠè¯•éªŒï¼Œç”³åŠžè€…应当ä¿è¯åœ¨ä¸´åºŠè¯•éªŒå‰å·²åˆ¶å®šæ–‡ä»¶ï¼Œæ˜Žç¡®åè°ƒç ”ç©¶è€…å’Œå…¶ä»–ç ”ç©¶è€…çš„èŒè´£åˆ†å·¥ã€‚
第五åä¸ƒæ¡ å¯¹äºŽå¤šä¸å¿ƒä¸´åºŠè¯•éªŒï¼Œç”³åŠžè€…åº”å½“æŒ‰ç…§ä¸´åºŠè¯•éªŒæ–¹æ¡ˆç»„ç»‡åˆ¶å®šæ ‡å‡†æ“作规程,并组织对å‚ä¸Žè¯•éªŒçš„æ‰€æœ‰ç ”ç©¶è€…è¿›è¡Œä¸´åºŠè¯•éªŒæ–¹æ¡ˆå’Œè¯•éªŒç”¨åŒ»ç–—å™¨æ¢°ä½¿ç”¨å’Œç»´æŠ¤çš„åŸ¹è®ï¼Œç¡®ä¿åœ¨ä¸´åºŠè¯•éªŒæ–¹æ¡ˆæ‰§è¡Œã€è¯•éªŒç”¨åŒ»ç–—器械使用方é¢çš„一致性。
第五åå…«æ¡ åœ¨å¤šä¸å¿ƒä¸´åºŠè¯•éªŒä¸ï¼Œç”³åŠžè€…应当ä¿è¯ç—…例报告表的设计严谨åˆç†ï¼Œèƒ½å¤Ÿä½¿åè°ƒç ”ç©¶è€…èŽ·å¾—å„分ä¸å¿ƒä¸´åºŠè¯•éªŒæœºæž„的所有数æ®ã€‚
ç¬¬ä¸ƒç« ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…èŒè´£
Oscarï¼šâ€œä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…èŒè´£â€å…±äºŒå一æ¡ï¼Œæ˜¯å¯¹ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…çš„èŒè´£è¦æ±‚ã€‚è§„å®šäº†ç ”ç©¶è€…çš„èµ„æ ¼æ¡ä»¶ï¼Œæ˜Žç¡®äº†ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åœ¨è¯•éªŒå‰ã€è¿‡ç¨‹ä¸ã€è¯•éªŒåŽçš„èŒè´£ï¼Œé‡ç‚¹æå‡ºç ”ç©¶è€…åº”é‡‡å–有关措施,ä¿æŠ¤å—试者的生命和å¥åº·ï¼Œç»´æŠ¤å—试者的æƒåˆ©ã€‚ã€
第五åä¹æ¡ 临床试验机构在接å—临床试验å‰ï¼Œåº”å½“æ ¹æ®è¯•éªŒç”¨åŒ»ç–—器械的特性,对相关资æºè¿›è¡Œè¯„估,以决定是å¦æŽ¥å—该临床试验。
第å…åæ¡ ä¸´åºŠè¯•éªŒæœºæž„åº”å½“æŒ‰ç…§ä¸Žç”³åŠžè€…çš„çº¦å®šå¦¥å–„ä¿å˜ä¸´åºŠè¯•éªŒè®°å½•å’ŒåŸºæœ¬æ–‡ä»¶ã€‚
第å…åä¸€æ¡ è´Ÿè´£ä¸´åºŠè¯•éªŒçš„ç ”ç©¶è€…åº”å½“å…·å¤‡ä¸‹åˆ—æ¡ä»¶ï¼š
(一)在该临床试验机构ä¸å…·æœ‰å‰¯ä¸»ä»»åŒ»å¸ˆã€å‰¯æ•™æŽˆã€å‰¯ç ”究员ç‰å‰¯é«˜çº§ä»¥ä¸Šç›¸å…³ä¸“业技术èŒç§°å’Œèµ„质;
(二)具有试验用医疗器械所è¦æ±‚的专业知识和ç»éªŒï¼Œå¿…è¦æ—¶åº”当ç»è¿‡æœ‰å…³åŸ¹è®ï¼›
(三)熟悉申办者è¦æ±‚和其所æ供的与临床试验有关的资料ã€æ–‡çŒ®ï¼›
(四)有能力åè°ƒã€æ”¯é…和使用进行该项试验的人员和设备,且有能力处ç†è¯•éªŒç”¨åŒ»ç–—器械å‘生的ä¸è‰¯äº‹ä»¶å’Œå…¶ä»–å…³è”事件;
(五)熟悉国家有关法律ã€æ³•è§„以åŠæœ¬è§„范。
第å…åäºŒæ¡ ä¸´åºŠè¯•éªŒå‰ï¼Œä¸´åºŠè¯•éªŒæœºæž„的医疗器械临床试验管ç†éƒ¨é—¨åº”当é…åˆç”³åŠžè€…å‘伦ç†å§”员会æ出申请,并按照规定递交相关文件。
第å…åä¸‰æ¡ ç ”ç©¶è€…åº”å½“ç¡®ä¿å‚与试验的有关工作人员熟悉试验用医疗器械的原ç†ã€é€‚用范围ã€äº§å“性能ã€æ“作方法ã€å®‰è£…è¦æ±‚以åŠæŠ€æœ¯æŒ‡æ ‡ï¼Œäº†è§£è¯¥è¯•éªŒç”¨åŒ»ç–—器械的临床å‰ç ”究资料和安全性资料,掌æ¡ä¸´åºŠè¯•éªŒå¯èƒ½äº§ç”Ÿé£Žé™©çš„防范以åŠç´§æ€¥å¤„ç†æ–¹æ³•ã€‚
第å…åå››æ¡ ç ”ç©¶è€…åº”å½“ä¿è¯æ‰€æœ‰ä¸´åºŠè¯•éªŒå‚与人员充分了解临床试验方案ã€ç›¸å…³è§„定ã€è¯•éªŒç”¨åŒ»ç–—器械特性以åŠä¸Žä¸´åºŠè¯•éªŒç›¸å…³çš„èŒè´£ï¼Œå¹¶ç¡®ä¿æœ‰è¶³å¤Ÿæ•°é‡å¹¶ç¬¦åˆä¸´åºŠè¯•éªŒæ–¹æ¡ˆå…¥é€‰æ ‡å‡†çš„å—试者进入临床试验ã€ç¡®ä¿æœ‰è¶³å¤Ÿçš„时间在å议约定的试验期内,按照相关规定安全地实施和完æˆä¸´åºŠè¯•éªŒã€‚
Oscar:旧版本ä¸æ述了医疗机构åŠä¸´åºŠè¯•éªŒäººå‘˜çš„èŒè´£åŒ…括与实施者共åŒè®¾è®¡ã€åˆ¶å®šä¸´åºŠè¯•éªŒæ–¹æ¡ˆã€‚在新版的GCPä¸ï¼Œä¸å†æåŠä¸´åºŠè¯•éªŒæœºæž„æˆ–è€…ä¸´åºŠè¯•éªŒçš„ç ”ç©¶è€…å…±åŒè®¾è®¡åˆ¶å®šæ–¹æ¡ˆã€‚方案设计和制定的主è¦èŒè´£äº¤ç”±ç”³åŠžè€…è´Ÿè´£ï¼Œä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…ä¸»è¦è´Ÿè´£ä¸´åºŠè¯•éªŒç®¡ç†ã€ä¸´åºŠè¯•éªŒæ–¹æ¡ˆç†Ÿæ‚‰å’Œå®žæ–½åŠè®°å½•çš„èŒè´£ã€‚这与申办者(生产ä¼ä¸šï¼‰ä½œä¸ºäº§å“的安全和有效的责任主体的è¦æ±‚是一致的和åˆç†çš„。
第å…åäº”æ¡ ç ”ç©¶è€…åº”å½“ä¿è¯å°†è¯•éªŒç”¨åŒ»ç–—器械åªç”¨äºŽè¯¥ä¸´åºŠè¯•éªŒçš„å—试者,并ä¸å¾—收å–任何费用。
第å…åå…æ¡ ç ”ç©¶è€…åº”å½“ä¸¥æ ¼éµå¾ªä¸´åºŠè¯•éªŒæ–¹æ¡ˆï¼Œæœªç»ç”³åŠžè€…和伦ç†å§”员会的åŒæ„,或者未按照规定ç»å›½å®¶é£Ÿå“è¯å“监ç£ç®¡ç†æ€»å±€æ‰¹å‡†ï¼Œä¸å¾—å离方案或者实质性改å˜æ–¹æ¡ˆã€‚但在å—试者é¢ä¸´ç›´æŽ¥å±é™©ç‰éœ€è¦ç«‹å³æ¶ˆé™¤çš„紧急情况下,也å¯ä»¥äº‹åŽä»¥ä¹¦é¢å½¢å¼æŠ¥å‘Šã€‚
第å…åä¸ƒæ¡ ç ”ç©¶è€…è´Ÿè´£æ‹›å‹Ÿå—试者ã€ä¸Žå—试者或者其监护人谈è¯ã€‚ç ”ç©¶è€…æœ‰è´£ä»»å‘å—试者说明试验用医疗器械以åŠä¸´åºŠè¯•éªŒæœ‰å…³çš„详细情况,告知å—试者å¯èƒ½çš„å—益和已知的ã€å¯ä»¥é¢„è§çš„风险,并å–å¾—å—试者或者其监护人ç¾å—和注明日期的知情åŒæ„书。
第å…åå…«æ¡ ç ”ç©¶è€…æˆ–è€…å‚与试验的其他人员,ä¸åº”当强迫或者以其他ä¸æ£å½“æ–¹å¼è¯±ä½¿å—试者å‚åŠ è¯•éªŒã€‚
第å…åä¹æ¡ ç ”ç©¶è€…åœ¨ä¸´åºŠè¯•éªŒä¸å‘现试验用医疗器械预期以外的ä¸è‰¯äº‹ä»¶æ—¶ï¼Œåº”当和申办者共åŒå¯¹çŸ¥æƒ…åŒæ„书相关内容进行修改,按照相关工作程åºæŠ¥ä¼¦ç†å§”员会审查åŒæ„åŽï¼Œç”±å—å½±å“çš„å—试者或者其监护人对修改åŽçš„知情åŒæ„书进行é‡æ–°ç¾å确认。
第七åæ¡ ç ”ç©¶è€…è´Ÿè´£åšå‡ºä½œå‡ºä¸Žä¸´åºŠè¯•éªŒç›¸å…³çš„医疗决定,在å‘生与临床试验相关的ä¸è‰¯äº‹ä»¶æ—¶ï¼Œä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“ä¿è¯ä¸ºå—试者æ供足够ã€åŠæ—¶çš„治疗和处ç†ã€‚当å—试者出现并å‘疾病需è¦æ²»ç–—和处ç†æ—¶ï¼Œç ”究者应当åŠæ—¶å‘ŠçŸ¥å—试者。
第七åä¸€æ¡ åœ¨ä¸´åºŠè¯•éªŒä¸å‡ºçŽ°ä¸¥é‡ä¸è‰¯äº‹ä»¶çš„ï¼Œç ”ç©¶è€…åº”å½“ç«‹å³å¯¹å—试者采å–适当的治疗措施,åŒæ—¶ä¹¦é¢æŠ¥å‘Šæ‰€å±žçš„临床试验机构医疗器械临床试验管ç†éƒ¨é—¨ï¼Œå¹¶ç»å…¶ä¹¦é¢é€šçŸ¥ç”³åŠžè€…。医疗器械临床试验管ç†éƒ¨é—¨åº”当在24å°æ—¶å†…书é¢æŠ¥å‘Šç›¸åº”的伦ç†å§”员会以åŠä¸´åºŠè¯•éªŒæœºæž„所在地çœã€è‡ªæ²»åŒºã€ç›´è¾–市食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨å’Œå«ç”Ÿè®¡ç”Ÿä¸»ç®¡éƒ¨é—¨ã€‚对于æ»äº¡äº‹ä»¶ï¼Œä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“å‘伦ç†å§”员会和申办者æ供所需è¦çš„全部资料。
第七åäºŒæ¡ ç ”ç©¶è€…åº”å½“è®°å½•ä¸´åºŠè¯•éªŒè¿‡ç¨‹ä¸å‘生的所有ä¸è‰¯äº‹ä»¶å’Œå‘现的器械缺陷,并与申办者共åŒåˆ†æžäº‹ä»¶åŽŸå› ,形æˆä¹¦é¢åˆ†æžæŠ¥å‘Šï¼Œæ出继ç»ã€æš‚åœæˆ–者终æ¢è¯•éªŒçš„æ„è§ï¼Œç»ä¸´åºŠè¯•éªŒæœºæž„医疗器械临床试验管ç†éƒ¨é—¨æŠ¥ä¼¦ç†å§”员会审查。
第七åä¸‰æ¡ ç ”ç©¶è€…åº”å½“ä¿è¯å°†ä¸´åºŠè¯•éªŒæ•°æ®å‡†ç¡®ã€å®Œæ•´ã€æ¸…æ™°ã€åŠæ—¶åœ°è½½å…¥ç—…ä¾‹æŠ¥å‘Šè¡¨ã€‚ç—…ä¾‹æŠ¥å‘Šè¡¨ç”±ç ”ç©¶è€…ç¾ç½²å§“å,任何数æ®çš„更改å‡åº”å½“ç”±ç ”ç©¶è€…ç¾åå¹¶æ ‡æ³¨æ—¥æœŸï¼ŒåŒæ—¶ä¿ç•™åŽŸå§‹è®°å½•ï¼ŒåŽŸå§‹è®°å½•åº”当清晰å¯è¾¨è¯†ã€‚
Oscar:临床数æ®è¦æ±‚准确清晰和åŠæ—¶åœ°è½½å…¥ç—…例报告表ä¸ï¼Œæ•°æ®ä¿®æ”¹æœ‰ç ”究者ç¾åå¹¶æ ‡æ³¨æ—¥æœŸï¼ŒåŽŸå§‹è®°å½•æ¸…æ™°å¯è¾¨ã€‚这是常规的质é‡ç®¡ç†ä½“系的GMPçš„è¦æ±‚。
第七åå››æ¡ ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“ç¡®ä¿ä¸´åºŠè¯•éªŒæ‰€å½¢æˆæ•°æ®ã€æ–‡ä»¶å’Œè®°å½•çš„真实ã€å‡†ç¡®ã€æ¸…æ™°ã€å®‰å…¨ã€‚
第七åäº”æ¡ ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“æŽ¥å—申办者的监查ã€æ ¸æŸ¥ä»¥åŠä¼¦ç†å§”员会的监ç£ï¼Œå¹¶æ供所需的与试验有关的全部记录。食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨ã€å«ç”Ÿè®¡ç”Ÿä¸»ç®¡éƒ¨é—¨æ´¾æ£€æŸ¥å‘˜å¼€å±•æ£€æŸ¥çš„, ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…åº”å½“äºˆä»¥é…åˆã€‚
Oscar:明确了食å“è¯å“åŠå«ç”Ÿè®¡ç”Ÿä¸»ç®¡éƒ¨é—¨æ£€æŸ¥çš„é…åˆè¦æ±‚。由于相关的临床试验已ç»é€šæŠ¥åˆ°ä¸´åºŠè¯•éªŒæœºæž„所在地的管ç†éƒ¨é—¨ï¼Œå› æ¤å¯¹äºŽé«˜é£Žé™©çš„产å“å’Œä¸¥æ ¼ç®¡æŽ§çš„äº§å“,éšæ—¶å˜åœ¨è¢«è¿™äº›éƒ¨é—¨æ£€æŸ¥çš„å¯èƒ½ã€‚
第七åå…æ¡ ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…å‘现风险超过å¯èƒ½çš„å—益,或者已ç»å¾—出足以判æ–试验用医疗器械安全性和有效性的结果ç‰ï¼Œéœ€è¦æš‚åœæˆ–者终æ¢ä¸´åºŠè¯•éªŒæ—¶ï¼Œåº”当通知å—试者,并ä¿è¯å—试者得到适当治疗和éšè®¿ï¼ŒåŒæ—¶æŒ‰ç…§è§„定报告,æ供详细书é¢è§£é‡Šã€‚å¿…è¦æ—¶ï¼ŒæŠ¥å‘Šæ‰€åœ¨åœ°çœã€è‡ªæ²»åŒºã€ç›´è¾–市食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨ã€‚
ç ”ç©¶è€…æŽ¥åˆ°ç”³åŠžè€…æˆ–è€…ä¼¦ç†å§”员会需è¦æš‚åœæˆ–者终æ¢ä¸´åºŠè¯•éªŒçš„通知时,应当åŠæ—¶é€šçŸ¥å—试者,并ä¿è¯å—试者得到适当治疗和éšè®¿ã€‚
第七åä¸ƒæ¡ ä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…å¯¹ç”³åŠžè€…è¿å有关规定或者è¦æ±‚改å˜è¯•éªŒæ•°æ®ã€ç»“论的,应当å‘申办者所在地çœã€è‡ªæ²»åŒºã€ç›´è¾–市食å“è¯å“监ç£ç®¡ç†éƒ¨é—¨æˆ–者国家食å“è¯å“监ç£ç®¡ç†æ€»å±€æŠ¥å‘Šã€‚
Oscar:对于申办者è¿åè§„å®šå®žæ–½ä¸´åºŠè¯•éªŒçš„ï¼Œä¸´åºŠè¯•éªŒæœºæž„å’Œç ”ç©¶è€…å°†å‘相关部门进行报告。
第七åå…«æ¡ ä¸´åºŠè¯•éªŒç»“æŸæ—¶ï¼Œç ”究者应当确ä¿å®Œæˆå„项记录ã€æŠ¥å‘Šã€‚åŒæ—¶ï¼Œç ”究者还应当确ä¿æ”¶åˆ°çš„试验用医疗器械与所使用的ã€åºŸå¼ƒçš„或者返还的数é‡ç›¸ç¬¦åˆï¼Œç¡®ä¿å‰©ä½™çš„试验用医疗器械妥善处ç†å¹¶è®°å½•å˜æ¡£ã€‚
Oscar:è¦æ±‚使用数é‡ã€åºŸå¼ƒæ•°é‡åŠè¿”还数é‡ç‰ç›¸ç¬¦ï¼Œæ‰€æœ‰å™¨æ¢°è¿½æº¯æ¸…楚。数é‡å¯¹ä¸ä¸Šä¹Ÿæ˜¯ä¸è¡Œçš„。
第七åä¹æ¡ ç ”ç©¶è€…å¯ä»¥æ ¹æ®ä¸´åºŠè¯•éªŒçš„需è¦ï¼ŒæŽˆæƒç›¸åº”人员进行å—试者招募ã€ä¸Žå—试者æŒç»æ²Ÿé€šã€ä¸´åºŠè¯•éªŒæ•°æ®è®°å½•ã€è¯•éªŒç”¨åŒ»ç–—器械管ç†ç‰ã€‚ç ”ç©¶è€…åº”å½“å¯¹å…¶æŽˆæƒçš„人员进行相关的培è®å¹¶å½¢æˆç›¸åº”的文件。
Oscar:本æ¡å…è®¸ç ”ç©¶è€…å¯ä»¥é€‚当的授æƒï¼Œå¯¹äºŽç ”究者的å¯æŽˆæƒèŒƒå›´åŠæŽˆæƒæµç¨‹å’Œè®°å½•äºˆä»¥è§„定。è¦æ³¨æ„ç ”ç©¶è€…çš„æŽˆæƒèŒƒå›´æ˜¯å¦è¶…出了本æ¡çš„规定?是å¦æœ‰ç›¸åº”的授æƒè®°å½•ï¼Ÿæ˜¯å¦æœ‰ç›¸å…³çš„培è®ï¼Ÿæ˜¯å¦æœ‰å½¢æˆç›¸åº”的文件?
ç¬¬å…«ç« è®°å½•ä¸ŽæŠ¥å‘Š
第八åæ¡ åœ¨ä¸´åºŠè¯•éªŒä¸ï¼Œç ”究者应当确ä¿å°†ä»»ä½•è§‚察与å‘现å‡æ£ç¡®å®Œæ•´åœ°äºˆä»¥è®°å½•ï¼Œå¹¶è®¤çœŸå¡«å†™ç—…例报告表。记录至少应当包括:
(一)所使用的试验用医疗器械的信æ¯ï¼ŒåŒ…括å称ã€åž‹å·ã€è§„æ ¼ã€æŽ¥æ”¶æ—¥æœŸã€æ‰¹å·æˆ–者系列å·ç‰ï¼›
(二)æ¯ä¸ªå—试者相关的病å²ä»¥åŠç—…情进展ç‰åŒ»ç–—记录ã€æŠ¤ç†è®°å½•ç‰ï¼›
(三)æ¯ä¸ªå—试者使用试验用医疗器械的记录,包括æ¯æ¬¡ä½¿ç”¨çš„日期ã€æ—¶é—´ã€è¯•éªŒç”¨åŒ»ç–—器械的状æ€ç‰ï¼›
(四)记录者的ç¾å以åŠæ—¥æœŸã€‚
Oscar:对于病例报告表åŠè®°å½•çš„è¦æ±‚。该部分内容是对于记录的新增内容,开展临床试验过程ä¸ï¼Œéœ€è¦å¯¹äºŽæœ¬ç« 节è¦æ±‚的记录进行仔细了解,以é¿å…临床试验开展真实,但是记录ä¸å®Œæ•´å¯¼è‡´è¢«åˆ¤æ–为ä¸çœŸå®žçš„被动情况。这些记录的è¦æ±‚å¯¹äºŽç›‘æŸ¥äººå‘˜å’Œæ ¸æŸ¥äººå‘˜æ¥è¯´ï¼Œæ˜¯å¿…须掌æ¡çš„。
第八åä¸€æ¡ ä¸´åºŠè¯•éªŒè®°å½•ä½œä¸ºåŽŸå§‹èµ„æ–™ï¼Œä¸å¾—éšæ„更改;确需作更改时应当说明ç†ç”±ï¼Œç¾å并注明日期。
对显著å离临床试验方案或者在临床å¯æŽ¥å—范围以外的数æ®åº”å½“åŠ ä»¥æ ¸å®žï¼Œç”±ç ”ç©¶è€…ä½œå¿…è¦çš„说明。
Oscar:记录的规范性相当é‡è¦ã€‚对于原始记录,如果进行éšæ„修改,å¯èƒ½å¯¼è‡´æ•°æ®ä¸çœŸå®žçš„å®¡æ ¸ç»“è®ºã€‚å› æ¤ï¼Œéœ€è¦æœ‰è‰¯å¥½çš„GDP(Good Document Practice良好文档实践)的è¦æ±‚,å³è‰¯å¥½çš„文档和记录规范æ¥æ”¯æŒã€‚
第八åäºŒæ¡ ç”³åŠžè€…åº”å½“å‡†ç¡®ã€å®Œæ•´åœ°è®°å½•ä¸Žä¸´åºŠè¯•éªŒç›¸å…³çš„ä¿¡æ¯ï¼Œå†…容包括:
(一)试验用医疗器械è¿é€å’Œå¤„ç†è®°å½•ï¼ŒåŒ…括å称ã€åž‹å·ã€è§„æ ¼ã€æ‰¹å·æˆ–者åºåˆ—å·ï¼ŒæŽ¥æ”¶äººçš„姓åã€åœ°å€ï¼Œè¿é€æ—¥æœŸï¼Œé€€å›žç»´ä¿®æˆ–者临床试验åŽåŒ»ç–—å™¨æ¢°æ ·å“回收与处置日期ã€åŽŸå› 和处ç†æ–¹æ³•ç‰ï¼›
(二)与临床试验机构ç¾è®¢çš„å议;
(三)监查报告ã€æ ¸æŸ¥æŠ¥å‘Šï¼›
(四)严é‡ä¸è‰¯äº‹ä»¶å’Œå¯èƒ½å¯¼è‡´ä¸¥é‡ä¸è‰¯äº‹ä»¶çš„器械缺陷的记录与报告。
Oscar:这些记录都需è¦è§„范记录。是临床监查人员CRA的必修课。
第八åä¸‰æ¡ ç ”ç©¶è€…åº”å½“æŒ‰ç…§ä¸´åºŠè¯•éªŒæ–¹æ¡ˆçš„è®¾è®¡è¦æ±‚,验è¯æˆ–者确认试验用医疗器械的安全性和有效性,并完æˆä¸´åºŠè¯•éªŒæŠ¥å‘Šã€‚多ä¸å¿ƒä¸´åºŠè¯•éªŒçš„临床试验报告应当包å«å„分ä¸å¿ƒçš„临床试验å°ç»“。
第八åå››æ¡ å¯¹äºŽå¤šä¸å¿ƒä¸´åºŠè¯•éªŒï¼Œå„分ä¸å¿ƒä¸´åºŠè¯•éªŒå°ç»“应当至少包括临床试验概况ã€ä¸´åºŠä¸€èˆ¬èµ„æ–™ã€è¯•éªŒç”¨åŒ»ç–—器械以åŠå¯¹ç…§ç”¨åŒ»ç–—器械的信æ¯æè¿°ã€å®‰å…¨æ€§å’Œæœ‰æ•ˆ
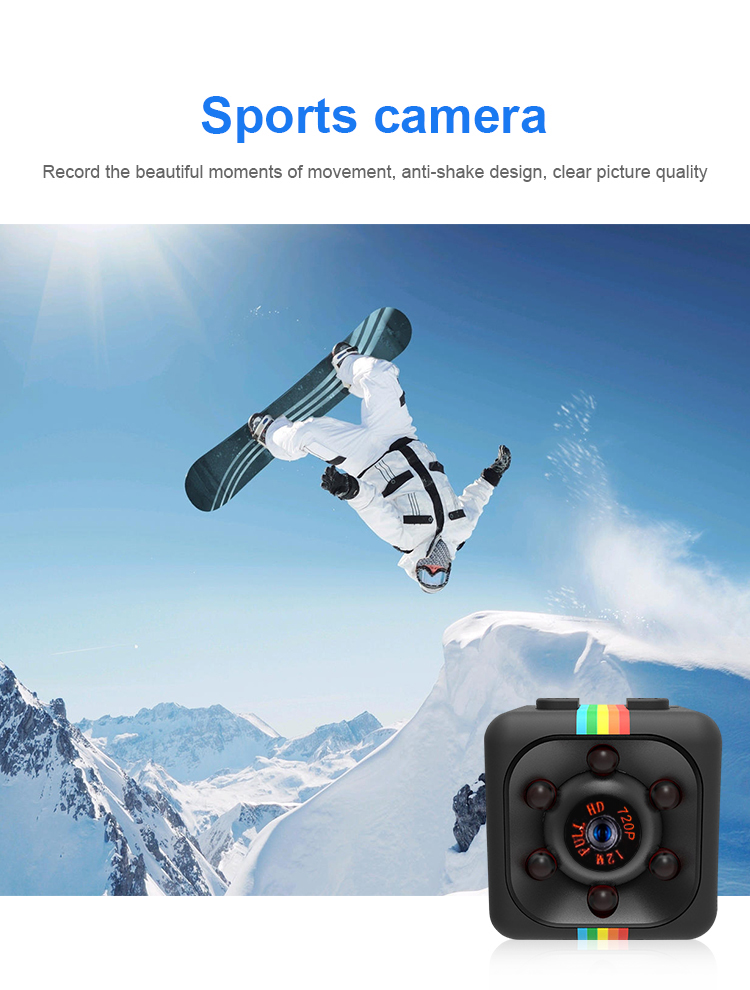
What is DVR Mini Camera
Dvr, which is called DigitalVideoRecorder in full, is a digital video recorder. Compared with traditional analog video recorders, dvr uses hard disk for recording, so it is often called hard disk recorder, also called DVR. It is a set of computer system for image computing, storage and processing. It has the functions of long-time video recording, recording, remote monitoring and control of images/voice and dynamic frames. DVR integrates five functions, including video recorder, picture splitter, PTZ lens control, alarm control, and network transmission. One device can replace a large number of devices in the analog monitoring system, Moreover, it has gradually gained advantages and popularity in terms of price.

The "digitalization" of DVR means that compression and storage technology is aimed at digital signals, rather than directly transmitting digitally encoded video images. Therefore, DVR must be deployed near the analog camera.
The function of DVR, with the increase of various voltage sensitive loads in the distribution network, puts forward higher requirements for power quality. However, due to system accidents in the power system, the voltage flicker, drop and other disturbances caused by the startup and shutdown of large equipment, lightning stroke and other principles are unavoidable. Moreover, in the current power grid, the ability to quickly restore power supply after power interruption is far from meeting the requirements of many sensitive loads. Therefore, it is necessary to provide users with stable and uninterrupted high-quality power when interference occurs. Dynamic voltage recovery (DVR) is the choice to solve the above problems today. DVR is connected in series to the feeder line that requires high-quality power to realize dynamic real-time voltage compensation for the line, so that the load end can get the desired high-quality power, and ensure the normal and uninterrupted operation of sensitive user equipment.
DVR Mini Camera,Cctv Camera System, Outdoor Waterproof NVR Set , Wireless Security Camera NVR, Cctv NVR Kit
DVR Mini Camera,Cctv Camera System, Outdoor Waterproof NVR Set , Wireless Security Camera NVR, Cctv NVR Kit
Shenzhen Fuvision Electronics Co., Ltd. , https://www.outdoorsolarcamera.com